Clare Roche started participating in Triathlons five years ago, but feared she may have to stop training when sudden pain on a regular run heralded the start of a hip problem.
Clare, who is in her 60s and lives near Wadhurst, has enjoyed a variety of sports from childhood. More recently she started to compete in Triathlons and has represented Great Britain in international competitions in her age group. One day whilst on a usual run, she developed severe pain and was unable to weight bear on her right leg. After hobbling home, things deteriorated quickly. She was unable to walk comfortably for any length of time and the night pain that radiated down the leg into the shin and ankle made sleeping difficult. Having to cancel her plans for a walking trip to the Himalayas, Clare made an appointment with her GP.
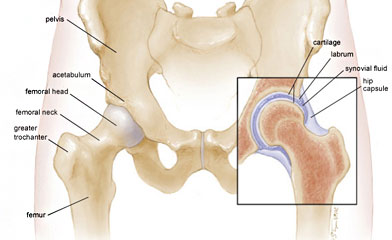
As a physiotherapist with over 40 years of experience in the Wadhurst area, she already knew that the problem was related to her hip. X-rays showed she had no articular cartilage left in the joint, and as a physiotherapist, she knew the only option was a hip replacement. Apart from her competitive sports she has a very busy family life with three children and an increasing number of grandchildren. Clare wanted to get back to training as soon as possible. She was keen to proceed quickly to prevent her muscle strength from deteriorating too dramatically. and decided to go privately.
She had witnessed great results in patients and friends following hip surgery performed by Mr Senthil Velayudham, Orthopaedic Hip Surgeon at Nuffield Health, Tunbridge Wells.
Following consultation with Mr Velayudham, he suggested a minimally invasive total hip replacement with ceramic on ceramic bearing surfaces was the way forward and her surgery was scheduled. A ‘total replacement’ means both parts of the joint are replaced – the ball and the socket.
The operation went well with no complications. For the first ten days Clare used crutches, after which she walked with a stick. At two to three weeks post-surgery she swam regularly and used an exercise bike. Within three-four weeks she walked unaided and could do about an hour of continuous walking. She was religious with her exercises, at home and in the gym, which helped her regain muscle strength; she is still doing them almost 18 months later. At around fourteen weeks after the operation, she began running and walking began, including short intervals of alternate slow jogging combined with brisk walking. Over the following weeks and months these exercises increased in duration and intensity. Four months after the operation, Clare went skiing with no problems. Seven months after her operation she was competing in a triathlon competition and nine months after came second in her first half ironman triathlon.
Prior to her operation Clare had gained a place to compete at the Triathlon World Championships in Lausanne at the beginning of September. She was worried she wouldn’t be fit enough to compete but at the end of August was on the starting line, less than a year following surgery.
In between competitions Clare enjoys her grandchildren, hiking, bird watching and conservation all of which are only possible with the pain free mobility that her new joint brings.
Mr Velayudham said: “Minimally invasive total hip replacement is a highly successful procedure helping patients return to good active lifestyle. Understanding patients’ expectation is very important. Using appropriate prostheses, restoring hip anatomy, preserving all the muscles controlling the hip and good rehabilitation helps patients to enjoy long good outcome following hip replacement.”
Claire added: “Having a surgeon who is not only technically excellent but someone who is empathetic to your situation and provides first-rate pre and post op oversight is crucial; Mr Velayudham more than fulfilled these criteria – as I knew he would having seen several of his patients over the years. Also impressive was the care I received at the Nuffield at all levels, from porters to senior medical staff. One hears horrible stories of waiting ages for a nurse when you really need them. That was not my experience; everyone was attentive and professional yet caring. The food was something special too.
“My advice to anyone who wants to get the most out of their joint replacement is firstly don’t leave it too long before having the operation, secondly try to choose a great surgeon like Mr V, and finally be serious and committed about exercises and general fitness both before your operation and for at least 12 month afterwards. We can all do more than we think we can!”