How do the implants work in a hip replacement?
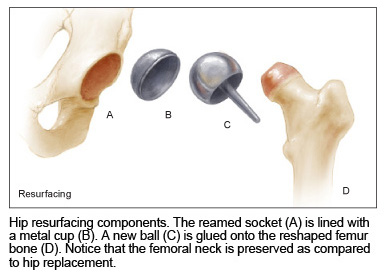
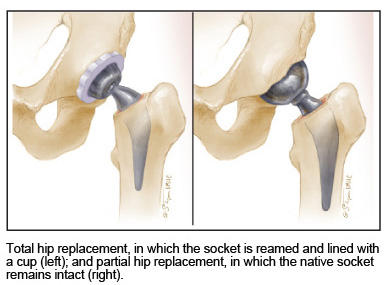
You have a natural socket (called the acetabulum) in the pelvis. The hip ball normally sits in this socket. By reaming away the damaged bone and cartilage, fresh bone is exposed, and a slightly oversized hemispherical socket made of a sturdy, inert titanium alloy is impacted into your bony socket. Usually this impaction does not require fixation with screws since the mechanical press-fit is snug enough. Into this titanium shell, a bearing surface of polyethylene, ceramic, or metal is then locked mechanically.
Next, the femur (thigh bone) is prepared by cutting off the arthritic femoral head (the ball of your hip joint). The cavity inside the femur bone is enlarged, and a slightly oversized femoral implant is securely impacted into the femur. The stem has a metal junction at its top end, designed to fit an artificial ball. This ball is made of a cobalt-chrome alloy, or ceramic, and matches the diameter of the bearing earlier fitted inside the artificial socket.
Once the ball is placed in the socket during surgery, the surgeon must adjust leg lengths, implant stability, muscle tension, and range of movement of the hip joint. This is where surgeon judgment and expertise are critical. The new artificial ball will rotate inside the synthetic shell just like a natural hip ball and socket would, except the artificial parts will not produce any pain.
What materials are used in a hip replacement or resurfacing?
The structural parts are made of titanium alloy. Structural means that the skeleton grows and bonds permanently to these parts. Alloy means that the metal is not pure titanium. It is a mixture of other metals to enhance the safety, performance, and avoid possible allergic reaction to any one metal.
Titanium alloys are used for this purpose because of durability, biocompatibility, several decades of experience, and the fact that titanium is less stiff than other metals and therefore better suited for skeletal reconstruction.

The bearings are mounted on the structural parts, using specially engineered tapers. Bearing surfaces in the hip are made of plastic, metal, or ceramic. The choice of bearing depends on the individual patient.
In engineering hip replacement components, the structural parts are optimized for their ability to bind to living bone and for long-term biocompatibility and durability, while the bearings are optimized for the lowest wear rates.
What do you do on the socket side of a hip replacement?
On the socket (pelvic) side of a hip replacement or resurfacing, a metal half-shell is fitted inside the patient’s own bony socket. Inside this shell, a locking mechanism fastens the bearing, which can be polyethylene, metal, or ceramic. Screws were once used to fix the socket to the pelvis bone, but with modern designs, screws are rarely necessary.
The bearing part can be changed even years down the road, without disturbing the metal cup that has grown into the pelvis.
What do you do on the femur side of a hip replacement?
On the femur (thigh bone) side, the inside cavity of the thighbone is enlarged, and a metal femoral stem is implanted in this cavity, where it will bind to the bone. On this stem, an artificial ball is attached using an engineering taper. The ball is made of either cobalt-chrome metal, or ceramic. The ball can be changed at any time in the future, if need be, without removing the stem from the femur.
What brand of hip implants do you use?
Brands such as Zimmer, OMNI, and Wright Medical Products have been popular in the past, but new ones are always being tested. Look for designs that have withstood the test of time, with excellent long-term results. Implant companies make several models and designs of implants, and the precise application depends on individual patient needs and anatomy.
The most common bearing surface used in hip replacements is a cobalt-chrome ball with a cross-linked polyethylene socket liner. This bearing is built upon decades of experience with standard (non cross-linked) polyethylene; the material offers more flexibility and options to make hip replacement safe and predictable.
If you have a strong preference for a certain type of joint prosthesis, or a certain type of material, discuss that with your surgeon.
There is very little difference between the implants offered by the major manufacturers. Be wary when companies pay doctors to promote or use any product.
What if I want a particular brand of hip replacement?
Simply let your surgeon know. You want to work with someone who embraces the latest technology, biomaterials, and surgical methods.
Be cautious about the unregulated marketing and promotion of hip and knee implants though. Orthopaedic companies and hospitals want business, and their advertisements rarely give the complete picture. Your surgeon should offer you unbiased opinion about different implants, while respecting whatever decision you make in this regard.
How much do the parts used in hip replacement weigh?
The parts weigh about 3 to 5 pounds. The bone removed during hip replacement weighs a little less. So, you may gain a few pounds of body weight as a result of hip replacement surgery. This is more than balanced by the fact that people tend to lose weight after surgery due to diminished appetite and the stress of an operation.
Why does an artificial hip wear?
Everything wears out over time. Artificial hip bearings are no exception. During everyday activity, our hips endure several million cycles a year. People who are athletic or walk more than usual will load their joints even more. Cyclic loading leads to wear, even though modern hip bearings are extremely wear-resistant. But, no bearing surface is completely wear-proof.
Realistically, for most patients, bearing wear in an artificial hip is not a practical concern. Assuming the surgery is done properly, most modern hip bearings will last longer than the patient’s lifespan.
Where do wear particles from the artificial hip go?
All hip bearings produce microscopic wear particles that collect in the soft tissue envelope around the artificial hip. This layer of tissue, called the hip capsule, forms around the prosthetic joint after surgery. Cells in this layer act like a “biological sink” by absorbing and storing the wear particles.
Some wear particles migrate into the body, and are spread by the circulating blood to remote organs such as the heart, liver, spleen, and lymph nodes. No study has shown any adverse impact of such wear particles from artificial hips that spread throughout the body, although this remains an area of investigation and research.
What is the advantage of ceramic bearings in hip replacement?
Ceramics are synthetic materials, used in industrial applications. When used in orthopaedic bearings, their wear rates are extremely low.
A disadvantage of ceramic bearings is that there are fewer options for the surgeon. This is related to engineering limitations. With future developments, ceramic bearing use may become more widespread. Today, for most patients, a cobalt-chrome ball and cross-linked polyethylene offers the best trade-offs between safety, longevity, flexibility, long-term wear, and sizing options.
Can ceramic parts be used in my hip replacement?
Yes, such as a ceramic ball and a plastic socket. Or we can use ceramics in both the ball and the socket. Either combination offers extreme wear resistance and durability.
Old-design ceramics were brittle, and the extreme hardness of ceramic materials limited their use in hip replacement. The newer ceramics are super tough alloys, especially engineered for the orthopaedic market. They are safer, and have excellent long-term outcomes, with almost zero wear.
Even newer ceramic materials made of silicon nitride are in development; silicon nitride offers even less wear, with extreme durability and strength.
When do you use cement to fix the hip components?
Cementing implants is reserved for the elderly and for cases in which the bone anatomy requires a cemented implant. The majority of hip replacements are done without bone cement.
In decades past, cement was used extensively to attach metal parts to bone. Cement is now rarely use cement in hip replacements thanks to developments in biomaterials and implant design.
How durable are cemented parts in hip replacement or resurfacing?
Data from hip replacements done many decades ago show that cemented total hip sockets usually loosened up after 10 to 15 years and that cemented femoral stems usually loosened up after 15 to 20 years. Today, cement is rarely used in hip replacements; in fact, if a previously cemented hip replacement has come loose, the parts used in repeat surgery are of a cementless design. Such components are designed to heal to native bone; this type of skeletal fixation has almost indefinite durability.
How do cementless hip implants attach to bone?
They attach by healing directly to bone. Metal surfaces are designed with a porous honeycomb metal structure, into which bone can grow. This biologic fixation is very strong and will not loosen over time.
While bone is growing into such parts, initial stability relies on a mechanical fit between metal and bone. This is achieved by physically impacting or hammering the parts into bone during surgery.
Once bone grows into the socket and femoral stem, the bond is permanent.
Can I get the same hip implant that a famous celebrity has?
Implant companies use celebrities to promote hip replacement, typically showing the youthful lifestyle and active involvement in skiing, golf, and other outdoor activities. Please view all marketing and promotional information with skepticism; such information is not always complete.
In reality, participation in sports such as golf and other activities is just as possible with one brand of hip components as the other. No brand in the market today is superior in terms of returning patients to activities faster or in giving patients an advantage in a specific sport, no matter which celebrity a company pays to tout its products.
Do I need a custom implant or instruments made from CT/MRI studies?
Hip components come in many sizes, configurations, models, and geometries. Off-shelf components give a precise fit in nearly all the patients. In some cases involving congenital abnormality, special-sized components can be ordered if necessary.
Technology keeps advancing, and in the future, custom-built hips that are designed precisely for one person to ensure perfect leg lengths, tissue tension, fit, and sizing will probably become a reality. Surgery advancements will probably mean that some patients may even be able to go home the day of surgery. These innovations reflect research and product development that professionals around the country are actively engaged in at the present time, to further improve on the already very successful operation of hip replacement.
Do you use human tissue or parts for hip replacement?
In routine total hip replacement, no such tissue is needed. Many years ago, we used allograft bone in some complicated cases to restore deficient bone. But with newer metal composites that can be shaped like bone, human tissue is no longer necessary for hip surgery.
In fact, metal augmentation techniques have advanced such that we can help patients who in the past were probably beyond help. The ability to rebuild hips that have had multiple operations previously, and to restore people to function, is a practical advantage of innovation and improvement in our health-care system.
Can patients develop an allergy to the artificial hip?
Such occurrences are exceedingly rare. Most commonly, what is often called an allergy is a missed, subtle infection. True metal allergies are usually well known to the patient ahead of time. In such unusual cases, it is possible to use components made of alternative metals, based on allergy testing, to which the patient is not sensitive.
Some patients did develop allergies and reactions to the metal-on-metal bearings; those designs have been recalled from the market.


 Osteotomy refers to cutting bone and realigning the leg, to relieve the pain of an arthritic hip. By altering biomechanics favorably, the loads across the ball and socket joint are lessened. Osteotomy was once a commonly used surgical option in young patients, back when hip replacements were not suitable for young and active people.
Osteotomy refers to cutting bone and realigning the leg, to relieve the pain of an arthritic hip. By altering biomechanics favorably, the loads across the ball and socket joint are lessened. Osteotomy was once a commonly used surgical option in young patients, back when hip replacements were not suitable for young and active people.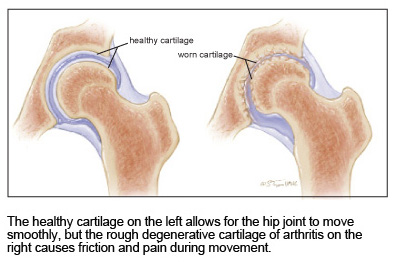 Muscles, tendons, and ligaments hold the ball in the socket, preventing it from slipping or dislocating. Hip dislocation, usually associated with severe physical trauma, is a serious condition requiring immediate medical treatment.
Muscles, tendons, and ligaments hold the ball in the socket, preventing it from slipping or dislocating. Hip dislocation, usually associated with severe physical trauma, is a serious condition requiring immediate medical treatment.