What are the “top ten things” I should know about knee replacement surgery?
 The following points apply to knee replacement surgery, no matter what implants are used, or how skilled your surgeon is.
The following points apply to knee replacement surgery, no matter what implants are used, or how skilled your surgeon is.
Knee surgery is not always the best option for knee pain or issues with walking.
Please keep in mind the following:
- Minimally invasive or not, knee surgery is painful. AVOID surgery if you can.
- Results from knee replacement depend critically on YOUR motivation, commitment, and participation.
- Proper PREPARATION for knee replacement will improve your outcome.
- Artificial knees can be NOISY; they sometimes pop, click, and clunk during movement.
- SWELLING, ACHING, and HEAT continue for longer than most people expect.
- Full recovery from knee replacement takes LONGER than most people think.
- Physical, family, emotional, and spiritual SUPPORT will help recovery after knee replacement.
- OLDER patients with knee arthritis will typically recover faster than younger patients; while this makes no sense, it is usually the case.
- If you cannot EXERCISE before and after surgery, avoid knee replacement surgery.



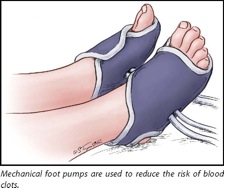 Mechanical foot pumps are used to squeeze the feet and ankles intermittently after surgery in order to help reduce the chances of a blood clot forming. These are useful while you will be in bed and resting. They are commonly used while you are in the hospital; you will not use them at home.
Mechanical foot pumps are used to squeeze the feet and ankles intermittently after surgery in order to help reduce the chances of a blood clot forming. These are useful while you will be in bed and resting. They are commonly used while you are in the hospital; you will not use them at home.