This information about possible complications is critical and should be reviewed by anyone contemplating hip or knee surgery of any kind.
This list will serve as the beginning point of our discussion about your surgery. This may be more detail than you want to know, but please take the time to read this material and understand it thoroughly.
 The odds of a complication occurring are very small. In the vast majority of surgical procedures, the outcomes are satisfactory; modern surgery is very safe. But, just as riding in a car or flying in an airplane, all risk cannot be eliminated.
The odds of a complication occurring are very small. In the vast majority of surgical procedures, the outcomes are satisfactory; modern surgery is very safe. But, just as riding in a car or flying in an airplane, all risk cannot be eliminated.
Therefore, it is vital that you review the material below, and ask questions, before any surgery is planned. Your surgeon and medical team will proceed with your surgery with the assumption that you understand, accept, and recognize this information.
If these risks are unacceptable, then please postpone the procedure. Bear in mind that although many complications are listed, all surgical procedures have a small chance of unpredictable outcomes — complications that no one can reasonably predict.
Some complications include:
- Blood Clots
- Pneumonia
- Nerve Injury
- Blood Vessel Injury
- Blood Transfusion Risks
- Anesthetic Complications
- Failure of Implants
- Heart Attack and Other Cardiac Complications
- Stroke
- Dislocation of the Components
- Infection
- Fracture
- Leg Length Inequality and Complications Related to Malalignment of the Leg
Your doctors will assume that you understand possible complications before embarking on surgery. More detailed information about the risks of hip or knee surgery can be found here.
Please understand that they may cancel a scheduled operation at any time up until the time of surgery if, in their judgment, you are unlikely to have a satisfactory result from the surgery or if the risk of a poor result or an adverse outcome exceeds their safe threshold for performing such surgery.

 Osteotomy refers to cutting bone and realigning the leg, to relieve the pain of an arthritic hip. By altering biomechanics favorably, the loads across the ball and socket joint are lessened. Osteotomy was once a commonly used surgical option in young patients, back when hip replacements were not suitable for young and active people.
Osteotomy refers to cutting bone and realigning the leg, to relieve the pain of an arthritic hip. By altering biomechanics favorably, the loads across the ball and socket joint are lessened. Osteotomy was once a commonly used surgical option in young patients, back when hip replacements were not suitable for young and active people.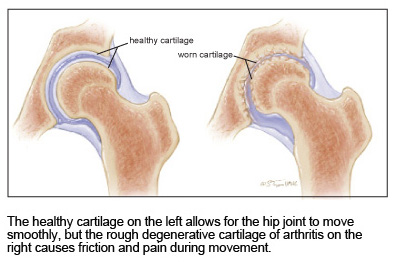 Muscles, tendons, and ligaments hold the ball in the socket, preventing it from slipping or dislocating. Hip dislocation, usually associated with severe physical trauma, is a serious condition requiring immediate medical treatment.
Muscles, tendons, and ligaments hold the ball in the socket, preventing it from slipping or dislocating. Hip dislocation, usually associated with severe physical trauma, is a serious condition requiring immediate medical treatment.